Ankylosing Spondylitis (AS) is a rheumatic condition that osteopaths cannot cure. We may be able to spot it though: diagnosis must be done by a rheumatologist, but symptoms are often missed in general practice. The average time between showing symptoms and receiving a diagnosis is 8.5 years. Early symptoms can seem very generic and be dismissed as non-specific lower back pain. Osteopaths are in a good position to flag unusual back pain like this as we see so many patients with lower back pain already.
What is Ankylosing Spondylitis?
AS is a condition of spinal inflammation and remodelling. During flares, the joints at the base of the spine and pelvis become inflamed. This can come with the symptoms of inflammation such as heat, pain, redness, and swelling. The daily pattern can be particularly telling: pain and stiffness after both rest, and intense exercise can suggest inflammation. This is even more likely if stiffness lasts more than half an hour.
The inflammatory episodes cause damage to the joints. This is because AS is autoimmune, meaning the body attacks itself. When the flare passes, the body tries to heal itself. Instead, it lays down new bone over the joint itself. This causes fusion over time, eventually leading to joint immobility and deformity. These joints are the areas most commonly affected, but AS also causes inflammation at the junctions between tendons and bones. The Achilles tendon is a common site for this enthesitis.
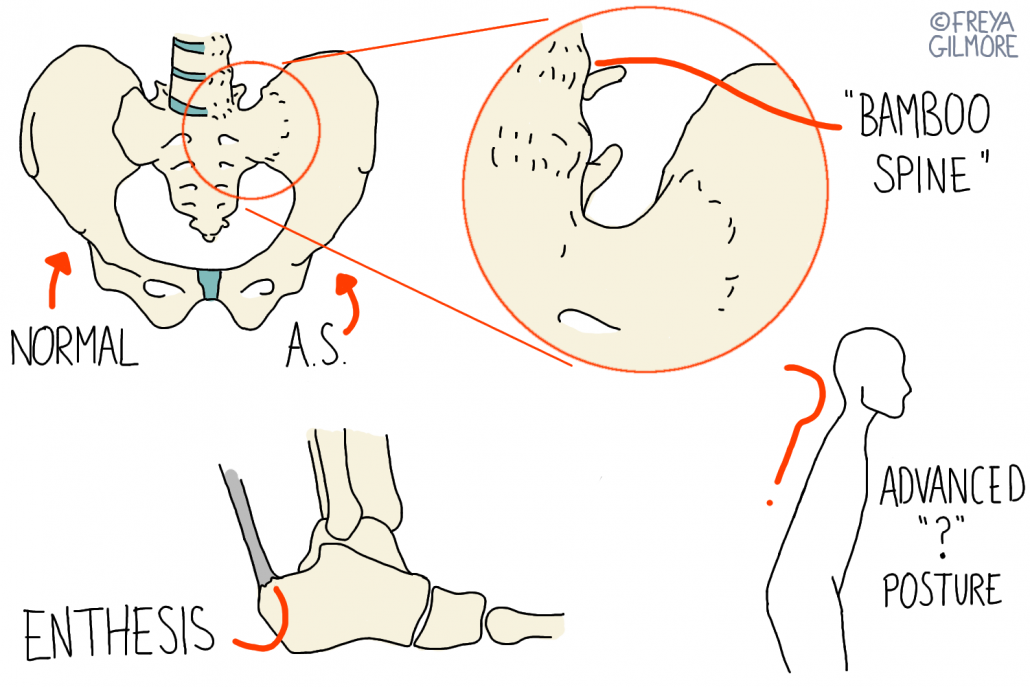
If left untreated, the repeated flare and fusion changes the posture. Previously AS was characterised by the “question mark posture” (illustrated above), but we know now that this is a sign of late stage AS. By this point, the changes have been made, and the disease will have burnt itself out, or be near to it. Identifying the symptoms of AS before this point is key. If we can act before fusion becomes significant, it may be possible to prevent the restrictions to some degree.
What If I Have Ankylosing Spondylitis?
Your osteopath cannot formally diagnose you, but they can refer you back to your GP with evidence to support a referral to rheumatology. Tools like the NHS questionnaire for clinicians can help here. Personal and family history can be useful in informing a decision. AS is related to other conditions like rheumatoid arthritis, ulcerative colitis, and Crohn’s disease. If your GP agrees that referral is necessary, you will be sent to rheumatology. Diagnosis may require blood tests and an MRI, which can also determine the severity of your case.
Your rheumatologist’s goal is to slow the disease progression. There are a number of drugs that can do this, and the right one for you depends on the way your AS is behaving. Stronger drugs, like DMARDs, can only be prescribed by a rheumatologist. This is a reason it is important to pursue the diagnosis if you suspect your back pain might be inflammatory.
Symptom Management
The most important parts of your treatment are a good exercise plan, and the appropriate medication. Your osteopath may be able to provide symptomatic relief and support your exercises. Gentle movement through the affected joints may give some relief, but your osteopath is less likely to click your back. We know that the new bone is more brittle than normal bone, and is therefore more prone to fracture. Strong treatment, like intense exercise, can aggravate your symptoms. Adversely, excess rest can make things worse too. Your osteopath will work with you to find the balance that helps you the most.
