The joints of the pelvis may be those that undergo the most dramatic changes in pregnancy. They certainly do during labour. By the third trimester, most pregnancies will have caused some pain in the lower back or pelvic joints, but sometimes this is more severe.
The Anatomy of the Pelvis
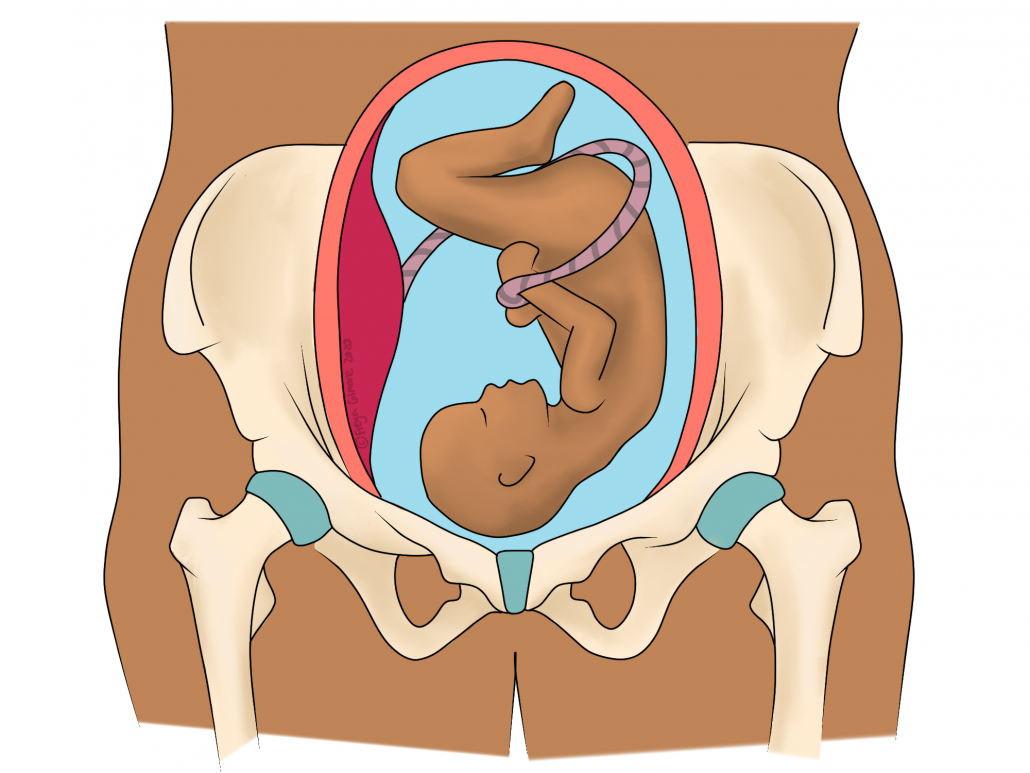
The pelvis is made of three bones and three joints. The two large bones are the inominates, which join at the front via the pubic symphysis. They also house the hip joints. The third bone is the sacrum, which is a large bone at the base of the spine. The joints on either side of the sacrum are the sacroiliac joints (SIJs).
Lots of strong muscles attach to the pelvic bones, such as the hamstrings, lower back muscles, and gluteal muscles. During pregnancy, when the centre of gravity shifts, these muscle groups are all asked to do more work. Therefore, they pull more on the pelvic bones. This relatively quick change can lead to pain through the pelvic joints. You can think of the three bones and joints as forming a ring: change in one area will affect the rest.
SPD: Symphysis Pubis Dysfunction
This diagnosis refers specifically to the joint at the front: the pubic symphysis. This joint has a large disc of cartilage in its centre, which makes it the most mobile of the three pelvic joints. Despite this, it is still not made for huge amounts of movement. During SPD, it can become irritated or even displaced.
SPD is the effect of instability within the pelvic ring. A significant factor in this is hormonal, which is unfortunately a necessary side effect of pregnancy. However, the symptoms may be managed with physical therapy. When a ligament is unable to perform its role alone, we can strengthen the muscles around it to help. Adversely, unmanaged SPD can severely restrict a patient’s ability to walk, and can also limit the options available to them during birth itself. It is not advised to adopt birthing positions in which the legs are open wide, as this can be painful and further injure the joint. Early intervention is important to minimise the risk of this scenario.
PGP: Pelvic Girdle Pain
This is quite a general term that encompasses SPD as well as SIJ pain. The SIJs typically act more as shock absorbers than joints of mobility, but during pregnancy they prepare for the motion required of them in childbirth. A hormone is produced from very early on in pregnancy, specifically with the role of relaxing off the large and strong ligaments around the SIJ. This new range of movement, combined with the new physical demands on the area, can cause pain within the joints.
The SIJs can also refer pain down the legs. Although sciatica is not an uncommon side effect of pregnancy, not all leg pain is down to a trapped nerve. With referred pain, the brain misinterprets the cause of an incoming pain signal. In the case of the SIJ, this may be misinterpreted as groin, calf, or thigh pain. Unlike sciatica, this is typically more of an ache than a sharp or shooting pain. It may also be accompanied by lower back pain.
Osteopathy and The Pelvis
Osteopaths work with the pelvis and lower back on a daily basis, and pregnancy does not need to be a barrier to treatment. If the pelvic joint in question is overloaded due to pregnancy changes on top of a pre-existing issue, we may be able to help. Just like upper back stiffness may go unnoticed until it causes pain in the neck, the same can be true for lower back or pelvic pain. Osteopaths look at the person as a whole and devise a personalised treatment plan.
Often a pre-existing problem is mild or asymptomatic before pregnancy, so for those trying to conceive, it may even be useful to visit your osteopath for a check-up before any problems do arise.
If you are developing pelvic girdle pain, book in now and start addressing it as soon as possible.

